-
开放科学(资源服务)标志码(OSID):

-
新型冠状病毒肺炎疫情(COVID-19)(以下简称“新冠肺炎疫情”)暴发以来,我国及时采取相应防控措施,严格限制居民出行,成功阻止了疫情的进一步蔓延. 有研究发现[1],COVID-19疫情对居民的主观幸福感产生了负面影响. 主观幸福感是反映个人身心健康的重要指标[2],受到日常行为活动(如身体活动情况以及睡眠质量等因素)的影响. 日常的体育活动可以通过降低焦虑和压力水平提高个体的主观幸福感[3],因此成为常用的干预消极情绪的手段之一[4]. 疫情期间,居民活动减少[5],且不同强度水平的活动(剧烈、中度、轻度)频率都有所下降,每天坐着的时间也从5 h增加到8 h[6]. 良好的睡眠习惯可以使个体增加积极的情绪体验,而积极情绪体验通过给个体带来较为平静、乐观的生活状态[7]从而增强个体的主观幸福感,睡眠质量是影响主观幸福感的重要因素[8]. 有调查显示,疫情期间居民们的睡眠—觉醒模式发生了改变[9],50%以上的居民存在入睡困难的情况并普遍存在晚睡(入睡时间平均滞后近1 h)的现象[10]. 此外,也有研究表明[11],缺乏运动或入睡时间推迟会使人们面临肥胖症、心血管疾病和神经性精神疾病的风险,而这些生理疾病会进一步降低人们的主观幸福感.
人格特质中,神经质与个体的情绪体验及睡眠质量密切相关[12-13]. 神经质与日常消极情绪体验呈正相关[14],与日常积极情绪体验呈负相关[15]. 此外,神经质人格对睡眠质量下降也有直接性的预测作用[16],有研究通过建立中介模型发现[10],疫情期间睡眠质量的下降取决于不同神经质人群所产生的负性情绪水平. 但是目前还没有研究探讨人格在入睡时间(晚睡)影响情绪体验过程中的作用机制.
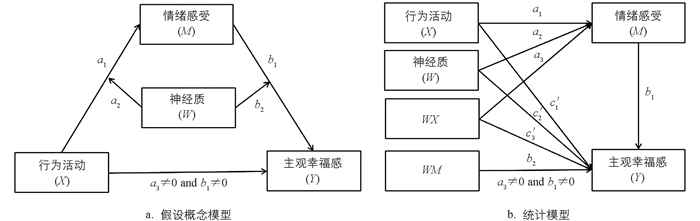
综上,本研究提出3点假设(图 1):假设1:体育运动和入睡时间都会影响居民主观幸福感(H1);假设2:情绪体验作为中介变量参与入睡时间对于主观幸福感的影响过程(H2);假设3:神经质作为调节变量参与日常活动影响情绪感受的过程或/并作为调节变量参与情绪体育影响主观幸福感的过程(H3).
HTML
-
于2020年2月17日至27日共招募75名参与者进行追踪研究,通过“问卷星”平台进行在线问卷调查,根据腕表数据剔除未正常佩戴者5人,根据每日问卷剔除未完整填写情绪状态者2人,最终获得有效数据共计68人.
-
本研究通过“问卷星”在线平台(www.wjx.cn)收集. 于2020年2月17日至2月27日收集相关数据,调查初期,参与者在线完成系统问卷,包括睡眠评估、饮食行为、情绪状态和活动情况的测量,同意参与该项目后签署知情同意书并进入纵向数据的追踪阶段.
将身体活动记录仪(wGT3X-BT,腕部佩戴)邮寄给参与者,并要求他们连续佩戴于惯用手5天5夜. 收到腕表当天即可开始佩戴,佩戴第二天算作数据采集的第一天. 参与者进入数据追踪阶段后需要于每个“追踪日”完成每日问卷,问卷内容包括当天的情绪状态以及前一天的睡眠情况.
-
该问卷为自编问卷,问卷包括性别、年龄、婚姻状况、当前工作状态、感染风险感知度等一般人口学变量.
-
采用Campbelt编制的幸福感指数量表[17],该量表采用1-7七级计分,得分越高表示对于生活满意度水平越高. 本研究中,该分量表的内部一致性系数为0.92.
-
采用Costa等编制[18],崔红等人修订[19]的简式大五人格量表(NEO-FFI)中的神经质分量表. 该量表包含12个题项(如“我常常觉得紧张或神经过敏”),采用5点计分(1=“非常不符合”至5=“非常符合”),得分越高,表示其神经质倾向越明显. 本研究中,该分量表的内部一致性系数为0.70.
-
该问卷为自编问卷,问卷包括积极情绪(共2题,分别测量乐观的、平静的情绪)和消极情绪(共5题,分别测量担忧的、无助的、恐惧的、悲伤的、愤怒的情绪). 题目采用5点计分(1=“完全没有”至5=“非常强烈”),得分越高,表示其当天该情绪体验越强烈. 每日问卷要求参与者在每天晚上20:00~21:00之间评价其当天是否体验到这种情绪以及该情绪的强烈程度. 本研究中,该每日量表第一天至第五天的内部一致性系数分别为0.75,0.83,0.80,0.81,0.82.
-
所有日间活动和夜间睡眠的客观测量参数均从身体活动记录仪中导出. wGT3X-BT活动记录仪[20]通过内置运动传感器以检测和记录运动情况. 以60 s为一个时间记录点,通过ActiLife软件(Version 19.2)生成参与者睡眠的简要统计数据. 一个记录点根据相邻点的活动计数的阈值来确定被划分为清醒或睡眠,该阈值遵循Cole-Kripke算法[21]. 身体活动记录仪得出的睡眠指数包括平均活动水平(计数)以及低、中、高、超高活动占比和入睡时间、清醒时间、睡眠中点、平均每日睡眠时间.
-
腕表数据使用ActiLife软件(Version 19.2)生成参与者睡眠的简要统计数据;使用SPSS 24.0进行描述性统计、相关性分析以及线性回归的检验;使用SPSS PROCESS 3.5进行中介模型的检验以及调节模型的建立.
1.1. 调查对象
1.2. 调查方法
1.3. 测量工具
1.3.1. 一般情况调查问卷
1.3.2. 主观幸福感测量问卷
1.3.3. 神经质问卷
1.3.4. 每日情绪问卷
1.3.5. 身体活动记录仪(wGT3X-BT)
1.4. 数据计算
-
参与本次追踪调查并完成5天数据追踪的有效人数共计68人,其中男性23人,女性45人;参与者年龄范围为31~60岁,平均年龄(47.53 ±5.42)岁;已婚者57人,未婚4人,离异7人. 本次调查的时间窗口中,未复工者47人,已复工者21人.
-
身体活动记录仪记录了参与者在疫情期间的活动计数和睡眠参数(表 1). 相关数据显示,参与者在此期间运动强度多为中低活动水平(>60%),平均身体活动水平(<1 700计步)在整体范围内偏低;其中32.2%的参与者平均活动值小于1 000计步,只有4.4%的参与者平均活动大于2 000计步.
疫情期间,参与者的平均睡眠中点均值在凌晨3点以后,其中有19.1%的参与者睡眠中点在凌晨3点之前,76.5%的参与者睡眠中点在凌晨3点至凌晨6点之间,4.4%的参与者睡眠中点在6点至9点之间. 参与者的平均每日入睡时间在23:53,其中有58.8%的参与者会在零点前入睡,41.2%的参与者在零点后入睡,只有一人的平均入睡时间在5:21;参与者的平均睡眠时长为8 h 12 min,其中14.7%的参与者睡眠不足7 h,30%的参与者每日睡眠平均时长为7~8 h,58.8%的参与者睡眠大于8 h(20.1%的参与者睡眠时长大于9 h),有2人的睡眠时长在10 h以上.
将参与者活动情况与其他心理变量进行相关分析发现,清醒活动均值(r=0.26,p<0.05)与居民主观幸福感显著正相关,与高活动占比(r=0.78,p<0.01)、超高活动占比显著正相关(r=0.83,p<0.01),与低活动占比显著负相关(r=-0.57,p<0.01),与消极情绪体验没有显著相关(r=-0.09,p=0.48).
将参与者睡眠情况与其他心理变量进行相关分析发现,入睡时间(r=-0.29,p<0.05)、清醒时间(r=-0.33,p<0.01)、睡眠中点时间(r=-0.34,p<0.01)均与其主观幸福感显著负相关;平均睡眠时长与其主观幸福感不存在显著相关(r=-0.08,p=0.54). 在睡眠指标中,只有入睡时间与积极情绪体验显著负相关(r=-0.25,p<0.05);积极情绪与主观幸福感显著正相关(r=0.63,p<0.01).
此外,清醒活动均值与入睡时间(r=-0.28,p<0.01)、清醒时间(r=-0.34,p<0.01)、睡眠中点(r=-0.34,p<0.01)均显著负相关;清醒时间与高活动(r=-0.38,p<0.01)、超高活动(r=-0.37,p<0.01)均显著负相关.
温忠麟等的研究[22]认为,消极情绪体验与活动均值、主观幸福感均不存在显著相关,不符合做中介检验的前提条件;入睡时间、积极情绪体验、主观幸福感3个变量相关显著,符合做中介检验的前提条件;积极情绪体验与神经质相关不显著(r=0.03,p=0.53)说明两变量具有相对独立性,适合后续进行神经质对于积极情绪体验影响主观幸福感的调节效应检[23].
-
以身体活动均值和入睡时间为自变量,以居民主观幸福感为因变量,分别代入线性回归方程(表 2).
活动均值(β=0.002,p<0.05)和入睡时间(β=-0.25,p<0.05)分别作自变量,主观幸福感作因变量时,均能显著预测居民主观幸福感,故假设1成立.
-
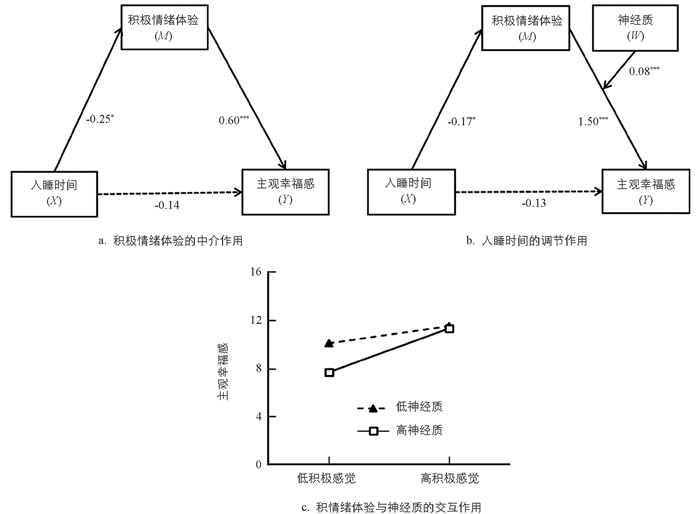
参考Hayes等[24]、叶宝娟等[25]的观点,使用SPSS 24.0中线性回归检验积极情绪在入睡时间与主观幸福感之间的中介作用(表 3),结果显示:当入睡时间为自变量,主观幸福感为因变量时,入睡时间能显著预测主观幸福感(β=-0.29,p<0.05);当入睡时间为自变量,积极情绪体验为因变量时,入睡时间能显著预测积极情绪体验(β=-0.253,p<0.05);当入睡时间与积极情绪体验同时进入回归方程时,入睡时间对于主观幸福感的预测效应不显著(β=-0.14,p>0.05),积极情绪体验对于主观幸福感预测效应显著(β=0.60,p<0.001).
积极情绪体验未进入回归方程时,入睡时间对居民主观幸福感预测作用显著(β=-0.29,p<0.05),积极情绪体验与入睡时间共同进入回归方程时,入睡时间对居民主观幸福感的预测作用不显著(β=-0.14,p=0.15),因此积极情绪体验在入睡时间影响居民主观幸福感过程中起到完全中介作用,假设1成立(图 2a).
-
在进行有调节的中介模型检验之前,需要将所有变量标准化为Z分数,对性别和年龄进行控制. 采用SPSS 24.0宏程序PROCESS 3.5的模型7检验神经质的调节作用(表 4). 该模型中,积极情绪显著正向预测了主观幸福感(b1=1.50,p<0.00),二者交互作用项对情绪体验的预测作用不显著(a3=-0.01,p=0.54). 故假设2不成立.
参考叶宝娟等[25]提出的有调节的中介效应检验程序,本研究在明确了积极情绪体验在入睡时间与主观幸福感关系中的中介作用之后,发现确定神经质调节后半段路径(积极情绪体验→居民主观幸福)的条件必须满足:①入睡时间对积极情绪体验的主效应显著;②神经质与积极情绪感受交互项的效应显著.
在进行有调节的中介模型检验之前,需要将所有变量标准化为Z分数,对性别和年龄进行控制. 采用SPSS 24.0宏程序PROCESS 3.5的模型14检验神经质的调节作用(表 5). 该模型中,入睡时间显著正向预测了积极情绪体验(a1=-0.27,p<0.05),二者交互作用项对居民主观幸福感的预测作用显著(b2=0.08,p<0.00).
可见入睡时间与主观幸福感之间存在有调节的中介效应,入睡时间通过中介变量积极情绪体验与神经质的交互项影响主观幸福感,即入睡时间→积极情绪感受→主观幸福感关系的后半路径受到了神经质的调节[24-25]. 假设3成立(图 2b).
为了揭示神经质如何调节积极情绪体验与主观幸福感之间关系,依据Hayes等[24]的调节效应检验程序,绘制了积极情绪体验与神经质的交互作用图(图 2c),对该交互作用进行简单斜率检验[26],结果表明,对于高神经质人群,积极情绪感受水平会显著影响主观幸福感(β=2.06,p<0.001);对于低神经质人群,积极情绪感受对主观幸福感的影响不显著(β=0.94,p=0.054).
2.1. 人口统计特征描述
2.2. 描述统计与相关分析
2.3. 回归方程检验
2.4. 中介模型的建立
2.5. 有调节的中介模型的建立
-
本研究采用主观报告量表采集疫情封闭初期人们的心理状态,使用身体活动记录仪记录参与者在此期间的日常行为活动的客观数据,尝试将生理指标与心理情绪体验相结合预测主观幸福感,并根据神经质水平将参与者进行划分,探究人格因素如何影响主观幸福感.
-
研究发现,疫情期间活动均值高、高活动占比高的参与者,入睡时间和清醒时间推迟的可能性越小,这与相关文献结果相似[27],即活动参与情况与睡眠质量之间存在相关,且运动有益于改善睡眠质量,但是以高中生为对象的一项调查结果[28]发现,睡眠习惯不良的人心理状态不容乐观,故参与体育活动的积极性低下. 运动与睡眠的交互作用成为近年关注热点,但是还没有完整的机制给予其支持.
-
从身体活动记录仪数据可以看出,疫情期间的封闭措施使人们的日常行为、活动范围受到限制,活动以中低强度为主. 以往研究表明[29],中低强度的活动即可有效降低居民的焦虑和压力水平,从而提高主观幸福感,但是本研究中并未发现两者存在显著相关,这印证了体育活动具有情境性的观点,即同样的锻炼强度,在不同的锻炼情境之中对情绪作用不同[30]. 疫情封闭期间,活动受限会增加人们对体重和体型的担忧,降低对自我的掌控感,并对体育锻炼和睡眠模式产生负面影响[31-32]. 本研究结果发现只有高强度的活动与主观幸福感显著正相关,这可以从神经生物学的视角进行解释,即高强度运动会加速多巴胺的分泌,这种化学物质会强化个体的能力感和价值感,从而促使主观幸福感的提高[33].
-
参与者的睡眠中点较晚,睡眠时间充足,说明晚睡晚起的情况较为普遍. 睡眠时长与主观幸福感不存在显著相关,这进一步说明,即使睡眠充足(8 h以上),但晚睡晚起仍会影响主观幸福感. 而睡眠中点与客观睡眠时长不存在相关,故推测参与者的睡眠潜伏期延长,即使睡眠时间充足,疫情期间“晚睡”情况可能仍属于失眠.
-
主观幸福感通常是由积极情绪体验的增强和消极情绪体验的降低所决定的[34]. 本研究发现,参与者入睡时间对于主观幸福感的负向影响完全是其积极情绪体验的降低的作用,而低积极情绪与抑郁相关,高消极情绪与抑郁和焦虑相关[35],这与先前研究结果一致[36-37],即晚睡晚起与抑郁症状呈显著正相关,且对抑郁症状和抑郁症具有正向预测作用. 本研究结果发现消极情绪体验与积极情绪体验、入睡时间、主观幸福感均不存在相关,说明:①积极情绪体验的降低并不会增强消极情绪体验,积极体验与消极体验同时存在,这一点支持了积极和消极情绪体验对抑郁和焦虑的独立影响,特别是积极情绪体验降低与抑郁相关的观点[38];②入睡时间推迟直接影响的是积极情绪体验的降低——个体大脑皮层的活跃度降低,从而体验到更少的积极情绪,并难以识别自己的快乐情绪[39].
-
神经质只调节了积极情绪体验影响主观幸福感的过程,说明积极情绪体验的增强会显著提高高神经质人群的主观幸福感水平,而低神经质人群的主观幸福感水平本身处于稳定状态,不会因为不同的情绪体验而发生明显变化. 此外,本研究发现,神经质并不参与调节入睡时间影响积极情绪体验的过程,说明入睡时间的推迟会普遍降低居民的积极情绪体验.
-
首先,由于处于封城的特殊时期,无法大规模招募被试,导致身体活动记录仪数据收集样本量相对较小;其次,身体活动记录仪数据于疫情期间采集,无法确定参与者在疫情前的睡眠和活动情况;而仅根据身体活动记录仪无法判断参与者的睡眠潜伏期时长,故无法直接判断晚睡情况属于失眠还是昼夜节律紊乱.
3.1. 疫情期间活动情况与入睡时间
3.2. 疫情期间活动情况与居民主观幸福感
3.3. 疫情期间睡眠情况与主观幸福感
3.4. 入睡时间影响主观幸福感:积极情绪体验的完全中介作用
3.5. 神经质的调节作用
3.6. 本研究的不足
-
1) 身体活动会增强居民主观幸福感,晚睡会降低居民主观幸福感;
2) 晚睡通过降低居民的积极情绪体验从而降低其主观幸福感;
3) 积极情绪体验的增强对高神经质人群的主观幸福感提升效果更显著.





 DownLoad:
DownLoad: