-
近期研究发现,对于新发生的呼吸衰竭,经鼻高流量氧疗(high-flow nasal cannula oxygen therapy,HFNC)在病死率方面优于无创通气(noninvasive ventilation,NIV)和标准氧疗(standard oxygen)[1].文献[2]也指出,当重型、危重型患者接受标准氧疗后呼吸窘迫和(或)低氧血症无法缓解时,可考虑使用高流量鼻导管氧疗或无创通气.但重型新型冠状病毒肺炎(novel coronavirus pneumonia,NCP)患者多存在免疫功能受损,而在免疫功能低下的患者中,HFNC相对于标准氧疗的优势尚未得到证实[3-5]. ROX指数(rate-oxygenation index)可以很好地预测HFNC的疗效:治疗2 h后,ROX指数大于4.88提示有效,而12 h后仍小于3.85则提示治疗失败.有研究指出,可通过ROX指数预测HFNC治疗能否成功[6].但对于HFNC治疗时间大于12 h的重型NCP患者来说,治疗失败的风险尚不清楚.本研究对重庆市公共卫生医疗救治中心负压病区应用HFNC治疗重型NCP患者的临床效果进行了回顾性分析.
全文HTML
-
选取2020年1月24日-2月23日入住重庆市公共卫生医疗救治中心负压病区、符合重型NCP诊断标准并接受HFNC治疗的全部病例进行分析.重型NCP诊断标准符合文献[2],有发热、咳嗽等症状,具有典型的NCP影像学特征且新型冠状病毒核酸阳性,同时满足以下任何一条:①出现气促,呼吸频率(respiratory rate,RR)≥30次/分;②静息状态下,指脉氧饱和度(SaO2)≤93%;③动脉血氧分压(PaO2)/吸入氧浓度(FiO2)≤300 mmHg(1 mmHg=0.133 kPa).
-
通过电子病历数据库及微生物实验室数据库,回顾性收集全部研究对象的临床资料,包括:①一般项目患者年龄、性别、基础疾病、RR和SaO2;②辅助检查入科时,CD4+绝对值、PaO2和FiO2,并计算不同时间点的ROX指数(定义为SaO2/FiO2与RR的比值);③患者转归继续HFNC或给予NIV或有创机械通气(Invasive mechanical ventilation,IMV).
-
用SPSS 19.0统计软件处理数据,计量资料以平均数±标准差(x±s)表示,比较用t检验或重复测量设计的方差分析,然后对单因素分析结果有意义的因素采用Cox风险比例模型(cox proportional-hazardsmodel,也称Cox回归)进行分析,p<0.05为差异有统计学意义.
1.1. 研究对象
1.2. 资料收集
1.3. 数据处理
-
2020年1月24日-2月23日期间,入住重庆市公共卫生医疗救治中心负压病区、符合重型NCP诊断标准并接受HFNC治疗的病例共有20例(男性13例,女性7例),平均年龄55.5岁(36岁~77岁). 20例中,合并2型糖尿病者2例(10%),合并2型糖尿病及高血压病者1例(5%),合并2型糖尿病及肥胖且体重指数(body mass index,BMI)为35.1者1例(5%),合并高血压病者1例(5%),合并高血压病及肥胖且体重指数为34.6者1例(5%).
-
所有病例均接受抗病毒、免疫调节及对症支持治疗(如合并细菌感染则给予抗感染治疗),治疗前抽取桡动脉血进行血气分析. 20例患者均接受HFNC治疗,采用Optiflow高流量湿化氧疗系统(新西兰Fisher-Paykel公司).初设参数:加温湿化吸入气体37℃,流量50 L/min,FiO2 100%.若血氧饱和度(blood oxygen saturation,SpO2)≥92%,则逐渐调整FiO2.所有患者治疗时间均≥48 h,治疗过程中记录0,2,12 h患者的SpO2、RR和FiO2,并抽取桡动脉血进行血气分析.根据文献[2]要求,7例(35%)患者治疗后症状及氧合指数(oxygenation index,用P/F表示)改善,继续HFNC治疗,定义为HFNC治疗成功组;13例患者(65%)经治疗后症状无改善或出现加重或恶化,后改为NIV或IMV,定义为HFNC治疗失败组.两组患者在性别、年龄和基础疾病等一般资料方面差异无统计学意义(p>0.05),但HFNC治疗失败组平均年龄高于HFNC治疗成功组(分别为63.30岁和57.76岁).
-
两组患者初始呼吸频率、入院时CD4+绝对值、P/F、治疗前ROX指数、治疗后2 h ROX指数、治疗后12 h ROX指数比较见表 1.两组初始呼吸频率、CD4+绝对值、P/F、治疗前ROX指数、12 h ROX指数比较差异无统计学意义(p>0.05),但成功组SaO2、治疗后2 h ROX指数和治疗后12 h ROX指数显著高于失败组(p<0.05).
-
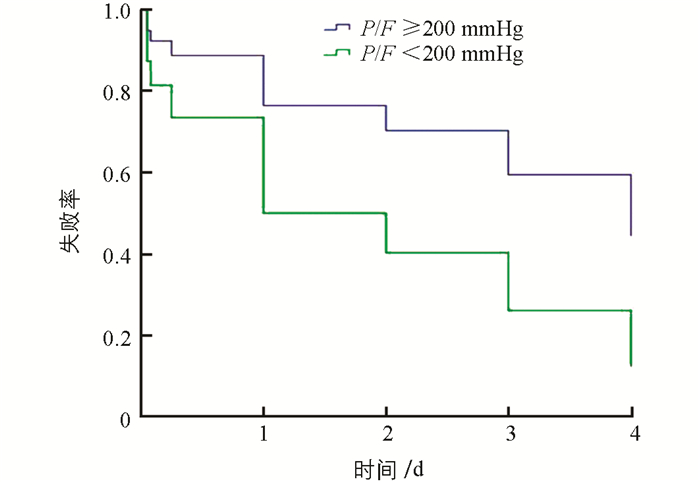
对表 1中p<0.05的因素如基线SaO2和治疗前、治疗后2 h及治疗后12 h的ROX指数,以及虽然p>0.05但观察中两组结果有明显差异的基线P/F用Cox风险比例模型进行分析,结果见表 2.基线SaO2、基线P/F和治疗后2 h、治疗后12 h的ROX指数均不是HFNC治疗失败的独立危险因素,但它们的值越低,HFNC治疗失败的风险就越大.基线P/F对HFNC治疗失败的风险预测见图 1,基线P/F<200 mmHg者,其HFNC治疗失败的风险高于基线P/F≥200 mmHg者.
2.1. 研究对象一般资料
2.2. 治疗方法与转归
2.3. HFNC治疗失败风险的单因素分析
2.4. HFNC治疗失败风险的多因素分析
-
新型冠状病毒属于β属的冠状病毒,人群普遍易感,以发热、干咳和乏力为主要表现,且在发病一周后出现呼吸困难和(或)低氧血症,严重者可迅速发展为急性呼吸窘迫综合征、脓毒症休克、难以纠正的代谢性酸中毒、出凝血功能障碍及多器官功能衰竭等.文献[2]指出,当患者接受标准氧疗后呼吸窘迫和(或)低氧血症无法缓解时,可考虑使用HFNC或NIV.但本研究收治的20名重型NCP患者绝大多数都表现为CD4+绝对值降低,提示免疫功能受损.在免疫功能低下的患者中,HFNC相对于标准氧疗的优势尚未得到证实.改善氧合作用对所有急性低氧性呼吸功能衰竭(acute hypoxemic respiratory failure,AHRF)都有意义,在免疫功能低下的患者中更是如此.这些患者的低氧血症更严重,根据文献[2],大多数患者都应给予HFNC治疗.但有研究表明,与标准氧疗相比,HFNC对于合并AHRF的免疫功能抑制患者并无显著获益[5].
对于急性I型呼吸衰竭的患者,不延误必要的气管插管呼吸机辅助呼吸时机是HFNC氧疗支持中的关键. Frat等[6]指出,当PaO2/FiO2<200 mmHg时,无创通气可以更好地预防严重低氧血症的发生.本研究对HNFC治疗重型NCP失败的患者基线P/F进行Cox风险比例模型性分析的结果也是如此.换言之,HFNC可作为合并轻度AHRF(P/F为200~300 mmHg)的NCP患者有效的救治手段. ROX指数能够很好地预测HFNC的疗效:治疗2 h后ROX指数大于4.88提示有效,而12 h后仍小于3.85则提示治疗失败. Roca O等[7]指出,在急性I型呼吸衰竭接受HFNC氧疗的过程中,ROX指数有助于判断患者是否需要气管插管呼吸机辅助呼吸的时机.因此,对于NCP合并急性呼吸窘迫综合征(acute respiratory distress syndrome,ARDS)的患者可用ROX指数筛选出风险很低和很高的那部分患者.本研究的单因素分析中成功组患者经HFNC治疗后2 h、12 h的ROX指数均大于失败组(p<0.05)也印证了这一点.
本研究为回顾性分析,即以现在为结果回溯过去的研究方法,由于条件限制较少,且样本量较小,易产生选择偏倚和回忆偏倚,也不能计算重型NCP患者HFNC治疗的成功率并直接计算相对危险度,故HFNC治疗重型NCP患者的疗效还有待进一步研究确证.



 下载:
下载: