-
2019年12月31日,我国报道了一组与湖北省武汉市华南海鲜批发市场相关人群中的肺炎病例[1]. 2020年1月7日,卫生部门证实了该病毒群与一种新型冠状病毒感染有关[2].尽管最初的报告病例与暴露于武汉海鲜市场有关,但目前的流行病学数据表明,该病毒可在人与人之间经呼吸道飞沫和接触传播,在相对封闭的环境中长时间暴露于高浓度气溶胶情况下存在经气溶胶传播的可能[3-7],主要侵犯人体呼吸系统.作为国际关注的突发公共卫生事件,其传染性强,人群普遍易感.全球有多个国家报道出现了新型冠状病毒肺炎(novel coronavirus pneumonia,NCP),截至2020年2月23日,我国感染人数已达77031人,治愈22746人(29.5%),死亡2444人(3.2%).作为一种新发的传染病,目前已有研究[8-9]报道了其临床特征及预后情况,但多数研究是对武汉当地住院患者的临床数据进行分析,对于武汉市以外其他地区感染者的临床特征及治疗预后情况报道较少.本研究分析了重庆地区NCP患者的流行病学史、临床表现、实验室检测结果、影像学特征、治疗方式和疗效,并对比分析了(危)重型患者与普通型/轻型患者在临床特征及预后方面的差异.
全文HTML
-
收集2020年1月24日-2020年2月23日重庆市公共卫生医疗救治中心收治的全部新型冠状病毒感染患者的资料,通过电子病历数据库及微生物实验室数据库,检索明确诊断为“新型冠状病毒感染”的病例,共223例患者纳入研究.所有临床研究结果(即出院、死亡率、住院时间)被监测至2020年2月23日,即为最后的随访日期.
-
新型冠状病毒的诊断标准:依据2020年2月18日国家卫生健康委员会印发的《新型冠状病毒肺炎诊疗方案》(试行第六版)[7]:
确诊病例:在疑似病例基础上,检查实时荧光RT-PCR检测新型冠状病毒核酸阳性或/和病毒基因测序,与已知的新型冠状病毒高度同源.
重型诊断标准:符合下列任何一条:①出现气促,RR≥30次/分;②静息状态下,指氧饱和度≤93%;③动脉血氧分压(PaO2)/吸氧浓度(FiO2)≤300 mm Hg,(1 mm Hg=0.133 kPa).
肺部影像学显示24~48 h内病灶明显进展>50%者按重型管理.
危重型诊断标准:符合以下情况之一者:①出现呼吸衰竭,且需要机械通气;②出现休克;③合并其他器官功能衰竭需ICU监护治疗.
-
符合新型冠状病毒肺炎诊断标准的病例按《新型冠状病毒肺炎诊疗方案》(试行第六版)[7]进行临床分型,将轻型和普通型分为一组即普通组,重型和危重型分为一组即重症组,比较两组(普通组和重症组)的基线特征、流行病学史、住院天数、发病至入院时间、临床表现(发热、咳嗽、呼吸困难、头痛、腹泻等)、实验室检验、胸部影像学表现及其临床转归等.
-
所有确诊患者均入住隔离病房或负压病房进行治疗,根据患者呼吸、指氧饱和度及氧合指数情况给予不同的氧疗措施,除常规对症及支持治疗外,均给予抗病毒治疗(包括α-干扰素、洛匹那韦/利托那韦、利巴韦林、阿比多尔、磷酸氯喹等). (危)重型患者在此治疗的基础上根据实际情况,经专家组讨论后部分还增加糖皮质激素、抗感染、恢复期血浆等治疗措施.
-
统计学分析采用SPSS 19.0软件,计数资料以频数(百分比)表示,组间比较采用卡方检验;正态分布的计量资料以x±s表示,组间比较采用独立样本t检验;偏态分布的计量资料以M(范围)表示,组间比较采用非参检验. p<0.05为差异有统计学意义.
1.1. 研究对象
1.2. 诊断标准
1.3. 研究方法
1.4. 治疗方案
1.5. 统计学分析
-
截至2020年2月23日,我院共收治NCP患者223例,平均年龄为(46.5±16.1)岁,男性106例,占47.5%.其中192例(86.1%)为轻型和普通型患者入住隔离病房,31例(13.9%)为(危)重型入住负压病房.流行病学史显示近2周内在本地接触过本地确诊患者、有武汉旅游或居住史、接触过来自武汉的确诊患者为主要感染途径,分别为76(34.1%)例、64(28.7%)例,40(17.9%)例.有24.2%(54/223)患者合并有慢性基础疾病,其中高血压(25例,11.2%)和糖尿病(18例,8.1%)是最常见的合并症(表 1).
普通组和重症组比较,两组在年龄、流行病学史、合并基础疾病方面差异均具有统计学意义(p<0.05).重症组患者平均年龄较大、合并基础疾病者较多,且更多的患者是因为接触来自武汉的新冠确诊患者而发病(表 1).
-
入组患者发病时最常见的症状为发热(119,53.4%)、咳嗽(113,50.7%),而头痛、肌痛、疲劳、腹泻和呼吸困难等症状较少见.与普通组比较,重症组发热患者较常见,且发热时以中高热为主,从发病到入院时间较普通组时间长,两组比较差异具有统计学意义(p<0.05).重症组中有15例出现呼吸困难,从发病到呼吸困难时间平均为(9.5±3.4)天.从病毒感染来源分析显示,重症组患者因接触武汉返渝人员而感染者明显多于普通组,而接触本地感染者及聚集性发病者在普通组较多,两组比较差异具有统计学意义(p<0.05)(表 2).
-
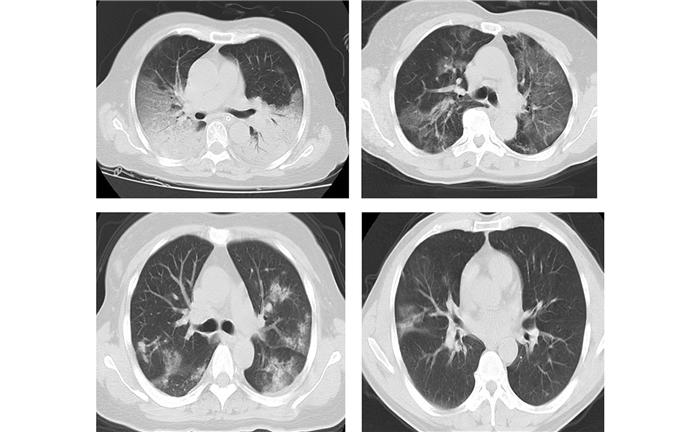
重症组与普通组患者在入院时的实验室检查结果存在较多差异(表 3),包括淋巴细胞计数、白蛋白、氧合指数偏低,丙氨酸氨基转移酶(ALT)、天门冬氨酸氨基转移酶(AST)、肌酸激酶(CK)、乳酸脱氢酶(LDH)、降钙素原(PCT)水平较普通组升高;且两组比较差异具有统计学意义(p<0.05).重症组患者D-二聚体明显升高,但两组比较差异不具有统计学意义(p>0.05). 223例入组病例中有87.9%(196/223)的患者胸部CT表现为双肺受累,单侧病变和无影像学改变分别占5.4%和6.7%;重症组均表现为双肺受累,普通组可积累双肺、单肺及无影像学改变;两组比较影像学在累及肺叶情况方面差异不具有统计学意义(p>0.05)(表 3、图 1).
-
223例NCP感染患者均接受了抗病毒治疗,抗病毒方案为1~3种抗病毒药物的组合.其中153(68.6%)例进行了氧疗,70(31.4%)例未接受氧气治疗者均为普通组患者;重症组患者除8(25.8%)例给予鼻导管吸氧外,其余23例(74.2%)患者分别给予了高流量、无创机械通气和有创机械通气治疗,两组在氧疗方式上的差异具有统计学意义(p<0.05).重症组有54.8%(17/31)的患者使用了小剂量(40~80) mg/天和短期(3~5)天的甲泼尼龙琥珀酸钠治疗(表 4).
截至2020年2月23日,仍有111例(49.8%%)患者在院,出院112例(50.2%),死亡0例.重症组出院患者平均住院天数明显长于普通组(p<0.05),但出院患者中两组患者在入院后核酸转阴时间差异不具有统计学意义(p>0.05).在院的20例重症组患者中,1例采用有创机械通气,2例已成功脱机拔管,5例采用无创机械通气治疗.
2.1. NCP患者的基本情况
2.2. 两组病例临床特征比较
2.3. 两组NCP患者实验室检查结果比较
2.4. 两组患者治疗方式及疗效比较
-
本研究显示入组的223例NCP患者平均年龄为46.5岁,男性占47.5%,31例(13.9%)发展为(危)重型.与普通型和轻型患者比较,发展为(危)重型患者的年龄较大,且有更多的慢性基础疾病;提示年龄和合并症可能是病情加重的危险因素.本研究数据病例显示男性和女性的发病率没有明显差异,而Chen[8]等研究报道NCP患者在男性中更多见,可能是既往报道的感染者多与武汉华南海鲜批发市场暴露有关,且感染者多为男性工人.本文病例的流行病学史显示重症组患者因接触武汉返渝人员而感染者明显多于普通组,而接触本地确诊患者而感染者及聚集性发病者在普通组多见,提示近2周内因接触来自武汉的确诊患者而发病者易发展为(危)重型,说明前几代病毒毒力可能强于后代病毒致病力.
本研究发现,NCP患者初期的典型症状主要是发热、咳嗽,而少数患者在发病时可出现头痛、肌痛、疲劳、腹泻等表现,甚至一些感染者可无任何不适,提示这些非典型的初始症状应该与更常见的症状一样得到重视,无症状携带者的存在需要引起足够的关注,相关接触者应尽快进行跟踪和隔离.在本文病例中,27例发热的(危)重型患者有81.5%(22/27)以中高热为主,且易出现呼吸频率加快和呼吸困难,其中出现呼吸困难的15例患者,从发病到出现呼吸困难的时间平均为(9.5±3.4)天,提示重型患者发病后如症状持续不缓解或影像学不吸收,需警惕发病10天左右进展为危重型.此外,本研究还发现重症组从发病到入院时间较普通组时间长,提示越晚入院治疗,发展为(危)重型的可能性越大.此类临床特征的出现可能有助于医生鉴别预后不良的患者.
在此项研究中还发现,常规外周血检查显示白细胞计数和淋巴细胞计数减少或正常,D-二聚体升高,且在(危)重型患者中更明显,这些都与之前报道的NCP患者相似[4].与普通组相比,重症组患者有更多的实验室指标检查异常,包括丙氨酸氨基转移酶(ALT)、天门冬氨酸氨基转移酶(AST)、肌酸激酶(CK)、乳酸脱氢酶(LDH)、降钙素原(PCT)水平明显升高,提示NCP感染可能与细胞免疫缺陷、肌原体损伤、肝损伤有关.而这些异常指标与之前在MERS-CoV和SARS-CoV感染患者中观察到的异常结果较相似[9].在这些患者中,87.9%(196/223)的感染者胸部CT表现为双肺受累,单侧病变和无影像学改变仅出现在普通型和轻型患者中,分别占5.4%(12/223)和6.7%(15/223);重症组均表现为双肺受累,早期胸部CT扫描多表现为多发小片状阴影及间质性改变,肺外区更为明显,这些阴影随后发展为双肺内的多个磨玻璃样病变,伴有浸润严重的病例可表现为“大白肺”或肺实变,继而出现呼吸困难,在一些严重病例中,可迅速发展为急性呼吸窘迫综合征、感染性休克、难治性代谢性酸中毒和凝血功能障碍等.
针对此次NCP感染,目前尚无疗效确切的抗病毒药物,但本文病例均给予抗病毒治疗,方案为1~3种不同抗病毒药物的组合,虽然抗病毒方案有所不同,但入院后至核酸转阴时间(平均为11.9天)在两组出院患者中无明显差异.除此之外,对于重症组患者我们还经验性地使用了糖皮质激素治疗.鉴于用于治疗SARS的大剂量糖皮质激素导致了严重的不良反应[10-11],但并没有有效降低冠状病毒感染的死亡率[12-14],我们对NCP感染的部分(危)重型患者使用了小剂量(40~80 mg/天)和短期(3~5天)的甲泼尼龙琥珀酸钠减轻肺部渗出,抑制全身细胞因子风暴,幸运的是本文患者预后均较好,而糖皮质激素是否发挥了重要作用尚需更多的临床数据来证实.在疾病的中后期,重症组患者可能会继发细菌甚至真菌感染.因此抗生素的合理使用应引起高度重视.除上述治疗外,入组的患者68.6%(153/223)接受了氧疗,根据病人的指氧饱和度和氧合指数情况选择了不同的氧疗方式.对于多数重症患者,早期无创通气可以改善患者的氧合指数;对于危重病人,应该及早考虑有创通气甚至体外膜肺氧合(ECMO).但到目前为止,入组的患者尚无人需要应用ECMO.在本研究中,严重缺氧和有创通气的总发生率低于之前的研究[4],可能与本地区的流行病学趋势有关,入组的病例中近50%患者为接触本地感染者或聚集而发病.
截至2020年2月23日,入组的NCP感染病例中已出院112例(50.2%),死亡0例,死亡率明显低于SARS的死亡率[9],但它的潜伏期较长,产生大量潜在的无症状携带者,对最终诊断和控制其传播造成一定的压力.
通过对重庆地区确诊的223例NCP感染病例的分析,初步确定了该地区的流行病学特点、疾病的主要临床特征和治疗原则. NCP患者通常以发热、咳嗽为首发症状,约14.3%的NCP患者易发展为(危)重型NCP;与普通组患者比较,重症组患者年龄更大、实验室检查结果更差.
然而,本研究为回顾性研究,(危)重型病例数相对较少,可能导致我们对这种疾病的认识存在一定的偏差.因此,研究结论尚待更大样本及前瞻性研究进一步证实.



 下载:
下载: