-
2019新型冠状病毒病(COVID-19)的爆发与传播,对我国居民的生命与健康造成了威胁.此次疫情是继2003年“非典”以来又一次突发性公共卫生事件.在以往的研究中,人们关注的重心多为医护人员在疫情期间睡眠的状况[1-2].此次疫情一方面构成重大情绪应激事件,增加了普通民众的抑郁、焦虑等情绪;另一方面,由于长期“禁足”在家,社会授时因子减弱,这些都大大增加了失眠的风险.本研究重点关注疫情期间普通居民的睡眠规律与身心健康.
我们选取了2020年2月17-2月27日作为调查窗口期.该时期全国确诊病例在70 548~78 497之间,疫情正处于平缓增长期.赵楠等[3]在疫情高峰期时表示,随着疫情的缓解,持续应激带来的心理健康问题在一定时期内可能越来越多地涌现出来,需要对后续长期心理援助与服务工作有所预案、逐步开展.武汉封城一个多月以来,由于各级政府防控人员和医务人员感染及呈现出的高强度工作状态,致使普通民众对新冠疫情经历了恐慌期和调整期.各地采取的封闭隔离、延迟开学等措施,以及不实消息的传播等因素导致恐惧、焦虑、抑郁和心理应激现象迅速增多[4]. Holmes等[5]将“改变个人当下持有的生活模式以适应生活环境变化的某个事件”定义为“生活事件”.新冠疫情完全符合上述特征,构成了一次重大的负性生活事件.
中国在本次疫情中采取了果断措施,限制出行,全民居家隔离.该过程正值春节假期,多数居民处于休假状态.大多数人本来就进入了晚睡晚起的度假模式,而居家隔离则进一步减弱了社会授时因子.前人研究发现,自然光暴露可以提高主观睡眠评价[6],而工作环境及相关的社会授时因子可提高人们的警觉度、认知表现和睡眠质量[7].黄庆玲等[8]研究发现,应激相关失眠易感性越高的人,更容易出现夜间觉醒等情况;常向东等[9]针对大学生群体的研究发现,睡眠质量与生活事件存在显著的正相关关系,说明个体经历的负性生活事件越多,其睡眠质量越差,即生活事件是影响大学生睡眠质量的重要因素之一.疫情这一负性生活事件势必会与居家隔离相叠加,严重影响到人们的睡眠健康.
如何针对居民个体特点进行有效的睡眠质量提升导引和睡眠障碍个性干预,是本研究的另一个目的.有研究发现,大五人格中的高神经质是睡眠不良(睡眠卫生差、睡眠质量差、嗜睡增加)的最佳预测因子[10].大五人格特质是作为稳定的心理特质对5-羟色胺起作用,以此参与调节睡眠节律[11].而疫情期间生活方式维度的变化则是非稳定的、非持久的[12].本研究要探讨这些非特质性变量在大五神经质对睡眠质量下降的直接关系中起着何种作用,从而为更有效的应对策略提供直接支持.
本研究通过问卷星平台,在全国发放问卷共1 122份. ①通过全体居民的疫情关注、情绪、饮食与睡眠等维度对生活方式进行描述性统计分析,以揭示疫情期间居民的日常作息规律. ②结合失眠的易感指标,特别对睡眠质量下降的原因进行了分析. ③发现了人格特质中的神经质和疫情期睡眠质量高度相关.进一步通过中介分析,获得了干预睡眠质量的核心变量.最后,本研究提出了一系列针对性的睡眠改善建议.
全文HTML
-
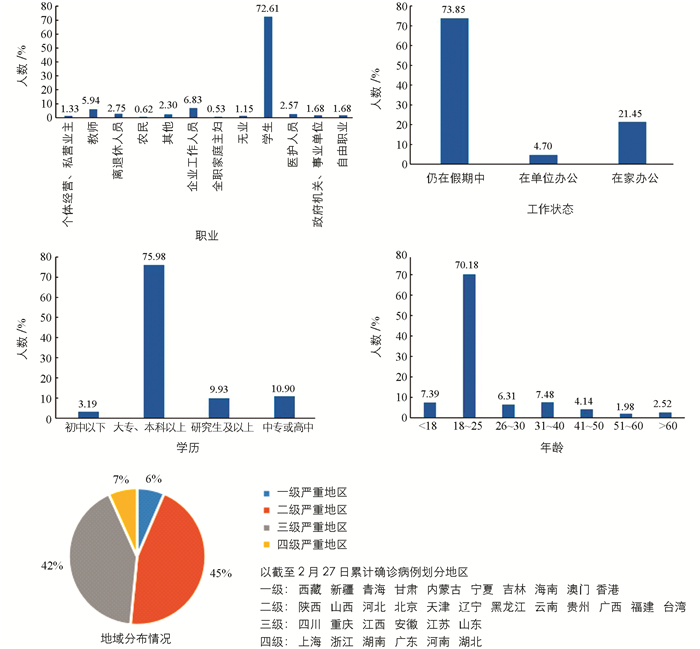
采取方便取样,以问卷星为平台发放问卷,内容主要包括日常饮食、睡眠作息等.采集时间为2020年2月17日-2月27日,共回收问卷1 122份,有效问卷1 066份,有效率为94.5%.其中,男性246人,女性876人;18~25岁的成年人群体是接受调查者的主体,占总数的70%;76%的居民具有大专及本科以上学历.具体的人口学信息和地域分布情况见图 1.本实验通过西南大学心理学部伦理委员会审核.
-
测量问卷共包括饮食、情绪和睡眠3个版块,共7个问卷,88道题目.
在居民饮食行为方面,采用课题组自制的疫情期间居民饮食行为调查量表.该量表包括17个项目,涉及居民的饮食行为和对特定食品的渴求等.在本研究中,该量表的CronBach α系数为0.85.
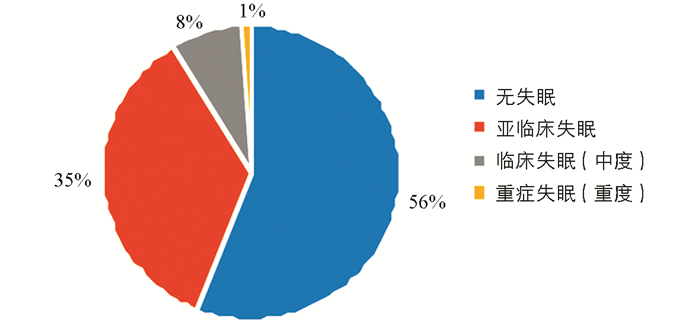
睡眠方面主要包括匹茨堡睡眠质量指数和失眠严重程度指数.匹茨堡睡眠质量指数由文献[13]编制.根据研究目的,本研究只采用了其中的部分指标.包括:①睡眠质量;②入睡时间;③睡眠时间;④睡眠效率.并且以2020年1月21日为时间界限,设置疫情前和疫情后两个时间跨度分别提问.失眠严重程度指数量表,采用文献[14]编制的版本.该量表共7个项目,采用0~4分5级计分,此次调查取用其中6个项目,总分在0~24之间.从总分划分失眠程度,0~6分表示“没有临床意义的失眠”,7~12分表示“亚临床失眠”,13~18分表示临床失眠(中度),18~24分表示“临床失眠(重度)”,该量表的CronBach α系数为0.84.
情绪方面涉及2个量表.情绪状态量表从压力、焦虑等9个维度对居民情绪状态进行评估.得分越高,负性情绪状态就越强.在本研究中,该量表的CronBach α系数为0.90.情绪调节问卷采用文献[15]编制的版本.该问卷共有10个项目,采用1~7计分,共分为2个维度:认知重评和表达抑制.各个维度得分越高,表明情绪调节策略的使用频率越高.
本研究还测量了居民的上网时间、疫情关注情况和人格特质等.其中人格特质部分采用大五人格神经质维度中文版问卷.该问卷包括12个项目,采用5级计分,得分越高表示神经质特质越明显.在本研究中,该量表的CronBach α系数为0.86.
1.1. 样本构成
1.2. 测量工具
-
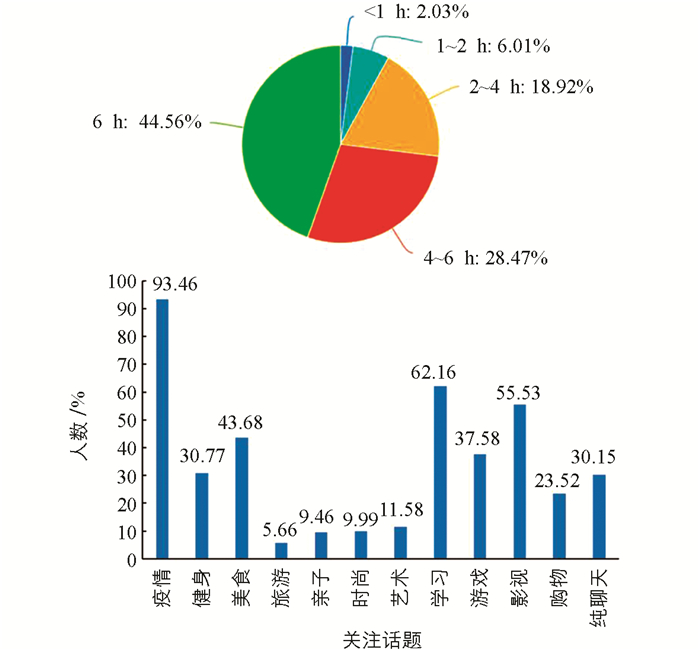
疫情发生以来,居民上网时间普遍较长,每天花在网上时间超过6 h的居民占此次调查人数的28.55%,每天上网时间4~6 h的居民占44.41%.在上网内容方面,90%以上的居民会每天主动关注疫情相关信息.微信、微博等新媒体的普遍使用,使此次疫情的相关信息更易获得、更能引起快速传播[16](图 2).
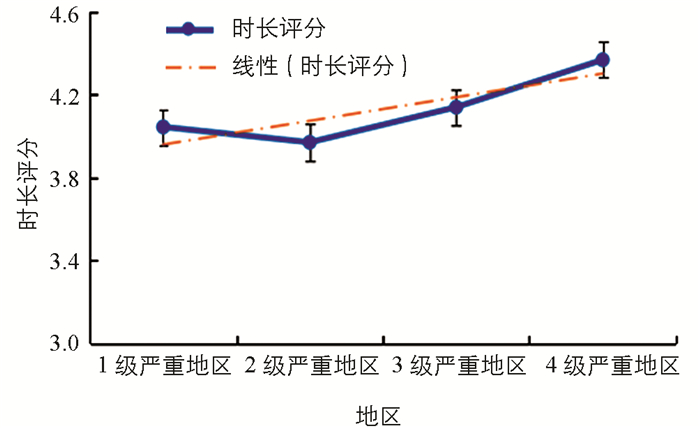
按照疫情严重程度,以本次疫情调查时间窗口中的2020年2月27日24时全国各省的累计确诊病例为标准,将地域划分为1~4级严重地区. 1级为最不严重地区,如青海等;4级为疫情极其严重地区,如湖北等.不同地域的居民上网关注疫情信息时长存在显著的差异(F=4.308,df=3,p < 0.01).疫情越严重的地区,居民上网关注疫情相关信息的时间越长,如图 3所示.其中最严重区域平均关注时长都在5 h以上.
-
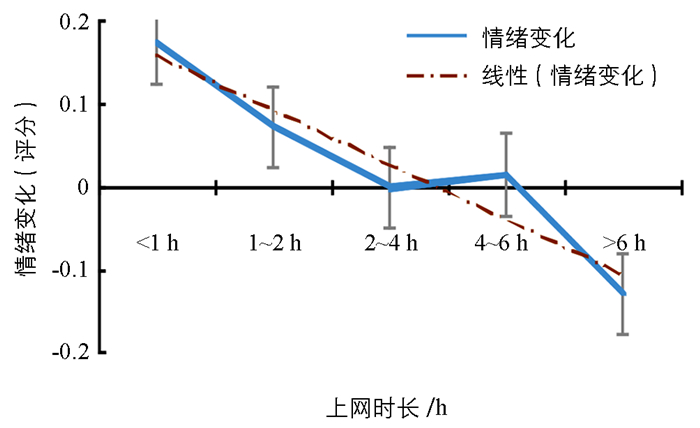
分析发现,上网关注疫情信息的时长与疫情信息带来的情绪影响呈显著负相关(r=-0.071,p=0.017).也就是说,上网关注疫情信息的时间越长,情绪状态就会越消极(图 4).
本研究将居民感受到的传染风险、生活满意度、消极情绪得分进行相关分析,发现自己或家人被传染的可能性与居民的消极情绪状态呈显著正相关(r=0.200,p < 0.01),与生活满意度呈显著负相关(r=-0.096,p < 0.001).也就是说,认为自己或家人被传染的风险越高,消极情绪越严重,生活满意度也越低.
-
疫情发生以来,有73.83%的居民会在情绪不好时渴望进食.分析发现,居民的情绪性进食与居民消极情绪呈显著正相关(r=0.23,p < 0.001),情绪状态越消极越容易发生情绪性进食.这一发现解释了疫情期间处于应激中的居民们对高热量食物的渴望普遍增加的现象.
居民的情绪性进食情况与食用高油、高盐、高糖食物(r=0.19,p < 0.001)以及使用零食(r=0.25,p < 0.001)的频率呈显著正相关,说明居民在发生情绪性进食时更偏向于选择高热量食物.
本研究中我们选择了在日常生活中常见的高热量食物为代表(奶茶、炸鸡、火锅),询问了对这些事物的渴求程度.结果显示,在疫情期间非常想喝奶茶、吃炸鸡、吃火锅的居民数量显著高于疫情前.表示愿意在疫情结束后第一时间去购买这些食物的居民数量都超过15%以上.
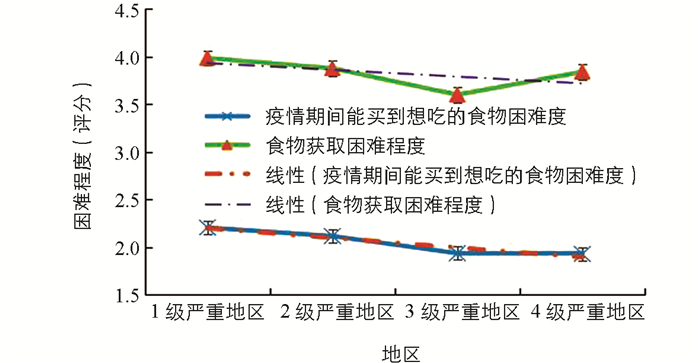
居民的饮食情况不仅取决于自身对各类食物的需求,也取决于在这段特殊时期内食物获取的困难程度.按疫情严重程度划分区域(图 5),居民们不仅感受到购买自己想吃的食物最为困难,且认为获取食物也最为困难.
通过相关分析可知,居民们买到自己想吃的食物的困难程度、食物获取的困难程度与出入小区的频率呈显著负相关,也就意味着出入频率越低,食物获取越困难(表 1).居民们的生活满意度与食物获取困难程度呈显著负相关,获取食物越困难,生活满意度越低.将饮食和睡眠情况共同分析得出结果,情绪性进食与做噩梦的频率、受睡眠影响的日间功能以及对睡眠问题的担忧程度均呈显著正相关.
-
从睡眠相关指数来看,居民在疫情后睡眠时长显著比疫情前要长(p < 0.001).普遍存在晚睡晚起的现象,平均滞后近1 h,平均多睡近0.5 h,但睡眠质量反而有下降.通过分析失眠严重程度指数(ISI)发现,疫情期间40%以上的居民都出现了失眠状况(图 6).并对失眠严重程度指数(ISI)的入睡困难、维持睡眠困难和早醒情况进行分析.结果发现,33.07%的居民报告有入睡困难;26.6%的居民报告有维持睡眠困难;24.2%的居民报告有早醒问题.
为何居民疫情期间睡眠时间更长,但睡眠质量却普遍下降了?基于这一问题,本研究结合生活方式维度相关变量的改变以及人格神经质维度等信息,对睡眠质量下降人群进行了进一步的分析.
-
通过对疫情期前后的睡眠质量进行对比分析,确定了存在睡眠质量下降现象的居民共有341人,占本次调查全体居民的32%.
本研究对睡眠质量下降人群疫情期前后基本睡眠指标的变化进行描述性分析.疫情期间,该人群的睡眠状况发生了较为明显的变化.我们从7组睡眠指标细化这些改变,分别是入睡时间、入睡潜伏期、起床时间、午睡时长、睡眠效率、睡眠中点、睡眠总时长.经配对样本t检验后发现,除了睡眠总时长,各指标疫情前后变化均极具有统计学意义(p < 0.001),具体变化情况如表 2所示.疫情期睡眠质量下降人群总体呈现出睡得更晚、更久的趋势.
-
该部分将生活方式各维度的变量与睡眠质量变化得分做相关分析,即从疫情关注、情绪变化、饮食、人格等维度指标,分析影响睡眠质量下降的因素.具体结果如下:
疫情信息导致情绪变化与睡眠质量变化得分呈显著负相关(r=-0.141,p=0.009),即疫情信息导致情绪越消极,疫情后的睡眠质量下降就越明显.
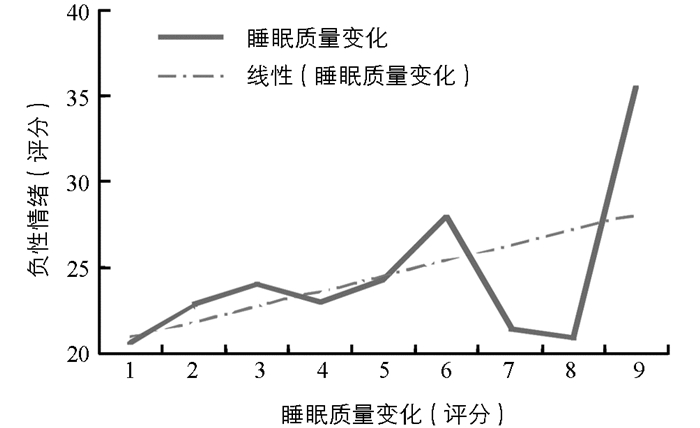
负性情绪与疫情后睡眠质量变化得分呈显著正相关(r=0.194,p < 0.001),这说明负性情绪得分越高,疫情后睡眠质量下降程度就越高,趋势如图 7所示.
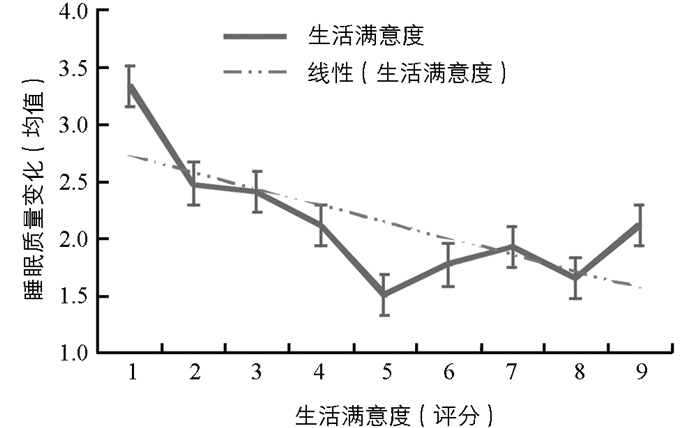
生活满意度与睡眠质量变化得分呈显著负相关(r=-0.268,p < 0.001),趋势如图 8所示,说明生活满意度越低,质量变化得分越高,即疫情后睡眠质量就越差.
大五人格神经质维度与睡眠质量下降得分之间有显著的正相关(r=0.128,p=0.02),即大五神经质得分越高,睡眠质量变化得分就越高,疫情后睡眠质量相较疫情前就越低.
-
有研究发现,大五人格特质作为重要的心理特质,对5-羟色胺有稳定作用,并影响睡眠[17].还有研究发现,大五人格的神经质维度对睡眠下降有直接性的预测作用[18].而疫情期间生活方式维度的改变则是应激性的、暂时的.基于上述原因,本研究尝试建立中介模型,即对睡眠起稳定作用的大五神经质维度作为预测变量,睡眠质量下降作为结果变量,探讨疫情期间生活方式维度的变量,是否在大五神经质维度与睡眠质量下降的关系中起着中介作用.
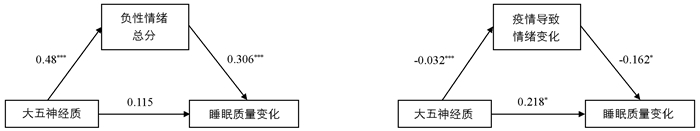
根据方杰等[19]的观点,本研究采用线性回归分析考查大五人格的神经质维度得分对睡眠质量变化得分的预测作用,结果显示,神经质维度得分对睡眠质量下降得分有显著的正向预测作用(B=0.027,t=2.507,p=0.013).加入其他变量作为中介变量发现,负性情绪总分在这两者间起完全中介作用(B=0.03,t=2.74,p=0.006,c=0.26,c′=0.115).中介效应值为0.015,95%的置信区间为[0.004,0.027],中介效应占总效应(0.026)的56%.另一方面,疫情导致情绪变化在神经质和睡眠质量的连接中起部分中介作用(B=0.16,t=-2.13,p=0.03,c=0.27,c′=0.218).中介效应值为0.005 2,95%的置信区间为[0.000 3,0.001 2],中介效应占总效应(0.027)的19%.居民生活方式改变维度的其他变量,都对神经质和睡眠质量变化关系没有显著的中介作用.负性情绪与疫情信息导致情绪变化作为中介变量的中介路径见图 9.
疫情期间产生的负性情绪在大五神经质维度与睡眠质量变化的关系中起完全中介作用,关注网上疫情信息产生的情绪变化在两者关系中起部分中介作用.
结合前面研究的部分结果,即情绪性进食与做噩梦的频率、受睡眠影响的日间功能以及对睡眠问题的担忧程度均呈显著正相关,以及情绪相关变量与睡眠质量下降群体的相关性,发现与情绪相关的因素对居民生活有多方面的影响.在疫情的心理干预中需重视情绪的作用,做好负性情绪的疏导工作.
2.1. 居民整体情绪、饮食和运动状况
2.1.1. 居民疫情关注时长
2.1.2. 居民情绪状态
2.1.3. 居民饮食与运动情况
2.2. 睡眠质量下降人群特征分析
2.2.1. 居民基本睡眠情况
2.2.2. 睡眠质量下降人群基本指标分析
2.2.3. 睡眠质量下降相关因素分析
2.2.4. 中介模型检验
-
当前,新冠疫情已经逐步得到控制,总体态势趋好,多省实现“零增长”.居民经过了疫情爆发期的社会应激和疫情平缓期的居家隔离,这些因素对生活仍有持续性影响,不可轻视.
本研究从疫情关注和情绪、饮食与睡眠等维度对居民的生活方式进行了描述性统计.结果发现,居民上网时间普遍较长,对疫情的关注度较高.疫情越严重的地区人们上网时间越长,情绪越倾向于消极.在饮食方面,居民的消极情绪会增加对高热量食物的选择和摄入,情绪性进食也增加了居民做噩梦的频率,影响居民日间功能,导致消极情绪增加,形成恶性循环.
在居民睡眠基本指标方面,对比疫情前都有显著变化.总体来看,较疫情前晚睡35 min,晚起42 min,总睡眠时长多27 min.并且,睡眠钟点平均延后55 min,这说明睡眠的昼夜节律变化十分明显.进一步从失眠人群占比、失眠具体指标上进行分析,发现失眠人数占总人数的44%,说明睡眠时间延长但睡眠质量反而更差.
为进一步调查疫情期睡眠质量变差的原因,本研究建立了中介模型,发现生活方式在神经质与疫情期睡眠质量之间起中介作用,揭示了大五人格的神经质维度对疫情期睡眠质量起直接的负向预测作用,与过去的研究结果相一致[18].进一步分析发现负性情绪、疫情导致情绪变化在模型中起着部分中介作用.
-
减少疫情期间手机的使用时间很有必要[20],尤其是夜间的使用时间. Munezawa等[21]的调查显示,熄灯后使用手机与睡眠障碍相关.疫情期间,夜间碎片时间更多,更可能关注疫情信息,导致负性情绪的产生.基于本研究在人格特质和睡眠质量上构建的中介模型,我们要特别关注人格特质上神经质较高的个体,他们需要更加注意情绪问题以及由此带来的睡眠障碍.
-
疫情期间禁足在家,增加了居民选用零食的可能性.零食作为一日三餐之外的额外加餐可以合理选用,但其热量不可忽略.考虑到社区封闭管理要求,通过小区内散步、室内运动等方式增加运动量是不错的选择.合理的进食量和运动是保持健康体质水平的基础.食物提供人体热量,运动消耗热量,如果进食过多而运动不足,多余的热量就会在体内以脂肪的形式积存下来,造成肥胖.
-
疫情期间睡眠质量下降需要引起足够认识.首先要对合理的睡眠有清晰的认知,包括正常的入睡时间、睡眠时长以及有利的睡眠环境.具体来说:①按时就寝,减少睡前电子设备的使用.睡前尽量不再看与疫情相关的新闻. ②睡眠时长方面尽量保证7~8 h的睡眠,过多或过少都不可取. ③规律作息,制定疫情期间有条理的运动、进食和就寝计划表,不仅有助于提高白天的学习和工作效率,对改善睡眠也有帮助.
4.1. 改善情绪
4.2. 改善进食与运动
4.3. 改善睡眠
-
本研究存在以下不足之处:①由于采用了方便取样,本研究的性别比例较不平衡,女性占大多数. ②本研究70%左右的样本为18~25岁的学生群体,全年龄的代表性不足. ③问卷是在2020年2月17-27日疫情平衡增长期收集的,此时居民大多已经适应隔离环境,应激反应有所减弱,使本研究难以推广到其他疫情时期. ④本次疫情心理援助的重点人群关注不足.这些人群包括新冠病毒病患者及家属、病亡者家属、特殊困难老年人等弱势群体、参与疫情防控的医务工作者、公安民警和社区工作者等一线工作人员.本研究在这些人群方面的样本较少.
本研究对普通居民疫情期间的生活方式、特别是睡眠状况进行了描述性统计,并提出相关建议,这对于普通居民在疫情逐渐进入平缓期后的生活具有一定的指导意义.并且,本研究发现人格特质对于睡眠质量下降有显著的预测作用,这一结果提示我们对具有神经质倾向人格的居民,要特别关注其睡眠问题.



 下载:
下载: