-
开放科学(资源服务)标识码(OSID):

-
化疗是目前肺癌晚期患者的主要治疗方法之一,但化疗药物对血管具有较大的刺激性,若是反复对静脉进行穿刺,可能会对外周静脉造成不可逆的损伤[1-2]。经外周静脉置入中心静脉导管(Peripherally inserted central catheter,PICC),通常可用于输注化疗药物及肠外营养药品,因其置管方便、安全性高、留置时间长等特点而广泛应用于癌症患者[3]。但长期留置PICC会对静脉壁产生机械摩擦,从而损伤血管壁,造成血流缓慢,激活内外源性凝血途径,使机体处于高凝状态,引起局部肿胀、不适、导管堵塞等,严重降低了治疗效果[4-6]。
预充式导管冲洗器是一种无针化、预充生理盐水的导管冲洗装置,其特色设计为活塞锁止环,可有效防止血液回流。相较于常用的传统手工导管冲洗法,预充式导管冲洗器不仅能避免医护人员直接接触导管发生感染,也能降低导管污染的风险。目前已有大量研究显示预充式导管冲洗器在降低中心静脉导管相关性血流感染的发生率中效果显著[7-8]。目前对癌症患者静脉置管后相关性血栓发生的影响及机制还不清楚,因此本研究拟探讨预充式导管冲洗对PICC置管后相关性静脉炎的发生情况及炎症和凝血相关因子的表达情况,以期为预防癌症患者PICC置管所引起静脉炎提供理论依据。
HTML
-
选取2021年6月至2022年1月在重庆大学附属肿瘤医院肿瘤放射治疗中心住院的肺癌晚期患者100例。所有患者均经病理及临床证实为肺癌晚期,预计纳入50例男性和50例女性,年龄为50~70岁。所有患者的Khorana评分均显示低风险。排除标准:1) 合并可能严重影响凝血功能的慢性肝、肾或其他疾病;2) 首次就诊时血小板PLT<1.0×1011/L或PLT>3..0×1011/L;3) 治疗过程中除PICC封管以外静脉或皮下使用过肝素的患者。
-
在肺癌患者化疗期间,给予常规护理,方法为:1) 定期为患者更换敷料;2) 严格遵守无菌操作规程,严格消毒;3) 定期观察患者穿刺部位有无出血渗血、渗液、贴膜卷边等异常情况,做好记录;4) 穿刺部位感染持续加重,要立即拔管处理,保障患者的生命安全。
所有患者随机分为2组:1) 传统手工冲洗PICC组(T组);2) 预充式导管冲洗器冲洗PICC组(MT组)。预充导管冲洗器冲洗方法为:每次0.5 s冲洗1 mL,暂停时间为0.5 s,然后冲洗0.4 s(90 mL/min,冲洗时间为9 s),直到推注结束。收集PICC置管前(Pre)、手冲式PICC置管后1 d(T1)、置管后30 d(T2)、置管后90 d(T3)以及预充式PICC置管后1 d(MT1)、置管后30 d(MT2)、置管后90 d(MT3)的空腹静脉血标本,储存在-20 ℃下备用。抽血前操作人员向患者详细说明本实验的目的及注意事项,签署患者知情同意书,保证患者权利。
-
1.2.2.1 经过相关专业培训且考核合格的护士观察相关性静脉炎,并对患者静脉炎情况进行评价,指标如下:
1) 阻塞:没有阻塞意味着可以抽血和注入液体;部分阻塞意味着无法抽回血液,但可以将液体注入静脉;完全阻塞意味着无法抽出回血且无法输注液体。
2) 静脉炎:按照美国输液护士协会(Intravenous nurses society,INS)的标准,判断静脉炎的发生与分级,等级为0~4级。
3) 渗出:按照INS的标准,判断渗出的发生与分级,等级为0~4级。
1.2.2.2 酶联免疫法(ELISA)检测血清中血栓相关因子血栓调节蛋白(TM)、抗凝血酶Ⅲ(ATⅢ)、血浆D-二聚体(D2D)、纤维蛋白原相关蛋白1(FGL1)以及炎症性细胞因子肿瘤坏死因子-α(TNF-α)、白介素-1β(IL-1β)水平。具体操作:用枸橼酸钠抗凝血采血管收集患者空腹血液标本2~3 mL,4 h内离心(1 000 r/min,5 min),分离血浆,分装后-20 ℃保存,实验时常温下溶解;采用ELISA测定后根据建立的标准曲线计算TM、ATⅢ、D2D、FGL1以及TNF-α、IL-1β的水平(OD值)。ELISA检测试剂盒均购自武汉酶免生物科技有限公司,实验条件及步骤均严格按照检测试剂盒说明书进行。
-
数据采用SPSS 17.0软件进行统计学分析,以x±s表示;多组间数据通过SPSS 20.0软件中的one-way ANOVA进行分析;组内两两比较采用t检验,p<0.05表示差异有统计学意义。
1.1. 资料来源
1.2. 方法
1.2.1. 分组
1.2.2. 指标检测
1.2.3. 统计学分析
-
结果见表 1。
-
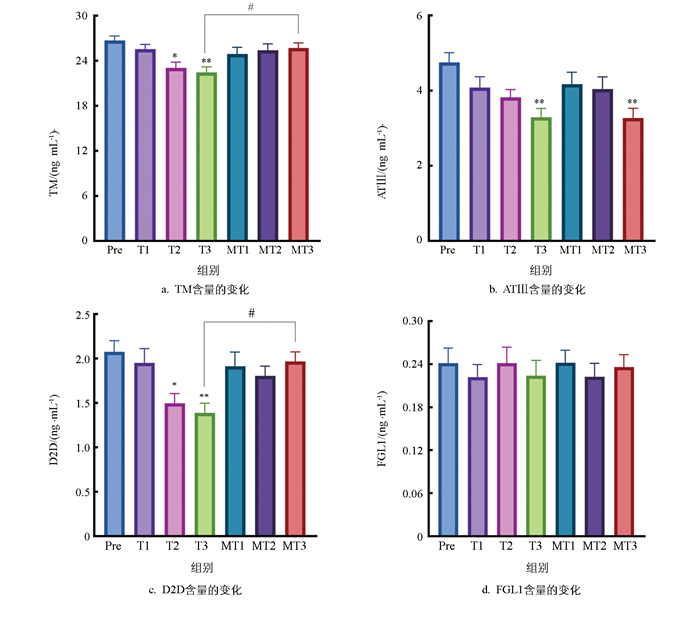
PICC置管后患者血清中TM的含量呈下降趋势(图 1a),相比于置管前(Pre组),T2组和T3组TM含量显著降低;使用预充式导管冲洗器能够有效阻止血清中TM含量的降低,其中MT3组相比于T3组TM含量显著上调(p<0.05)。血清中ATⅢ含量呈现下降趋势(图 1b),相比于置管前Pre组,手工冲洗90 d后(T3组)ATⅢ含量显著降低;预充式导管冲洗器的使用未改变PICC置管后血清中ATⅢ的含量,相比于Pre组,MT3组ATⅢ仍显著降低(p<0.01)。血清中D2D含量也呈下降趋势(图 1c),T2组和T3组D2D含量显著降低;而使用预充式导管冲洗器能够使血清中D2D含量维持在PICC置管前水平,相比于T3组,MT3组D2D含量显著上调(p<0.05)。血清中FGL1含量在PICC后无显著变化(图 1d)。
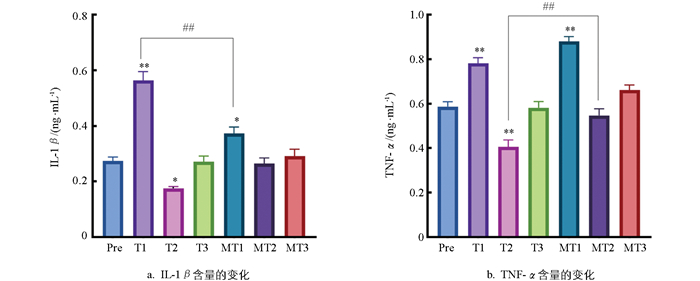
PICC置管后患者血清中IL-1β的含量具有波动性(图 2a),相比于置管前(Pre组),PICC置管后1 d(T1组)IL-1β呈显著上升趋势(p<0.01),T2组略有下降,T3组回归正常水平。相比于手工冲洗T1组,使用预充式导管冲洗器能够降低MT1组的IL-1β含量(p<0.01),对其他时间点影响不大。PICC置管后患者血清中TNF-α的变化与IL-1β基本相同(图 2b),相比于置管前(Pre组),PICC置管后1 d(T1组)TNF-α呈显著上升趋势(p<0.01),T2组略有下降,T3组回归正常水平。相比于手工冲洗T2组,预充式冲洗能够升高MT2组的TNF-α含量(p<0.01),对其他时间点影响不大。
2.1. PICC置管后患者血栓性静脉炎等级评价
2.2. 预充式导管冲洗器对PICC置管后血栓相关因子的影响
-
PICC给临床静脉输液治疗带来巨大便利的同时,也出现了一系列的并发症。PICC置入静脉血管后容易损伤相关静脉血管内皮,进而引起后续的阻塞、静脉炎和渗出等并发症,甚至引发导管相关性血栓[9]。研究显示,PICC导管相关性血栓发生率为3%~20%,无症状性血栓发生率为51.4%~61.9%[10]。PICC作为一种有创性的治疗方法,与患者的血栓形成有关。PICC由于穿刺时管路行程较长,操作过程中因动作过大容易损伤血管壁,伴随着血液高凝状态和血流缓慢,导致局部出现红肿和疼痛。目前临床上保持PICC通畅最有效的方法是依靠定期冲洗,通过冲洗可以加快导管周围的血流速度,以降低导管相关性血栓的发生率,但常用的传统手工配制冲管液及封管液的污染率达19%,可能引起导管相关性血流感染[11]。预充式导管冲洗器可减少医护人员的常规操作时间,降低医院内环境中革兰氏阳性菌的定植和污染风险[8]。
-
正常的血管内皮具有抗凝作用,一旦血管内皮发生损伤,易引起炎症及血栓的形成。血栓调节蛋白(TM)主要由血管内皮细胞生成,约99%以上的血管内皮细胞表达TM,辅助凝血酶激活蛋白C系统产生抗凝效果。TM释放入血成为sTM,而sTM是炎症反应或血管内皮细胞受损的重要标志蛋白[12]。抗凝血酶Ⅲ(ATⅢ)是体内重要的抗凝因子,控制着血液的凝固和纤维蛋白的溶解,ATⅢ水平降低表明血液抗凝活性减弱。血浆纤维蛋白原1(FGL1)是纤维蛋白的前体,在凝血的最后阶段,可溶性纤维蛋白原转变成不溶性纤维蛋白,使血液凝固。而血浆D-二聚体(D2D)是纤维蛋白降解后的特异性产物,测定血浆D-二聚体可以判断纤维蛋白是否已经生成,有助于了解凝血机能状态[13]。TM、ATⅢ、D2D的显著升高说明机体处于高凝状态,易形成静脉血栓。这不仅增加了肺癌患者PICC置管后血栓形成、导管堵塞、肺栓塞等风险,还会加重静脉炎与炎症反应,影响输液治疗、患者预后及生活质量。
静脉血栓是静脉的一种急性非化脓性炎症,并伴有继发性血栓形成的疾病。一方面肿瘤患者自身处于高凝状态,肿瘤细胞的内源性合成及单核巨噬细胞的抗肿瘤作用可以导致组织因子TNF-α的升高,直接激活凝血酶原,参与静脉血栓形成;另一方面导管作为异物在血管内漂浮移动,导管头端对血管壁的刺激、治疗过程中药物的刺激等,均会直接或间接地刺激静脉壁而引起局部血管内膜反应性炎症,引起炎症细胞因子的释放,从而导致血液中炎症细胞因子的增多[14-15]。IL-1β是一种典型的促炎细胞因子,能够诱导血管收缩,提高对血管活性物质的反应性,损害内皮依赖性血管舒张,这些效应可能参与血管痉挛,血栓形成[16-17]。通过检测患者血液中IL-1β的水平可以动态观察PICC置管后机体的炎症程度、预测血栓形成风险以及深入研究相关病理生理机制,可以作为PICC置管后评价静脉血栓形成的生物标记物。
本研究发现置管后明显增加了患者静脉炎和渗出的发生率。通过ELISA检测血样中血栓相关因子和炎症性细胞因子水平,发现较置管前(Pre组),不管是传统手工冲洗还是预充式导管冲洗,患者TM、ATⅢ及D2D水平显著降低,同时TNFα、IL-1β含量明显升高,且差异有统计学意义(p<0.01);而相较于手工冲洗,预充式导管冲洗器冲洗PICC后,静脉炎和渗出的发生率有所下降,同时IL-1β等显著降低,且差异有统计学意义(p<0.01),说明预充式导管冲洗器冲洗能明显降低PICC导致的患者血栓性静脉炎的发生,这与降低血栓相关因子和炎症相关因子有关,但具体机制还有待更深一步研究。
-
PICC插管后出现静脉炎和渗出,伴随着TM、ATⅢ及D2D水平显著降低以及TNF-α、IL-1β水平的升高,说明置管会导致静脉的慢性炎症。预充式导管冲洗器冲洗能明显逆转PICC导致的各项因子的变化,有效减少PICC导致的患者血栓性静脉炎的发生。本研究为PICC相关血栓性静脉炎的防治提供了新的思路与理论依据,有助于推动该领域进一步深入探究预充式导管冲洗器在不同置管场景及患者群体中的应用优化策略,也为后续研发更具针对性与高效性的静脉炎预防措施奠定基础。





 DownLoad:
DownLoad: